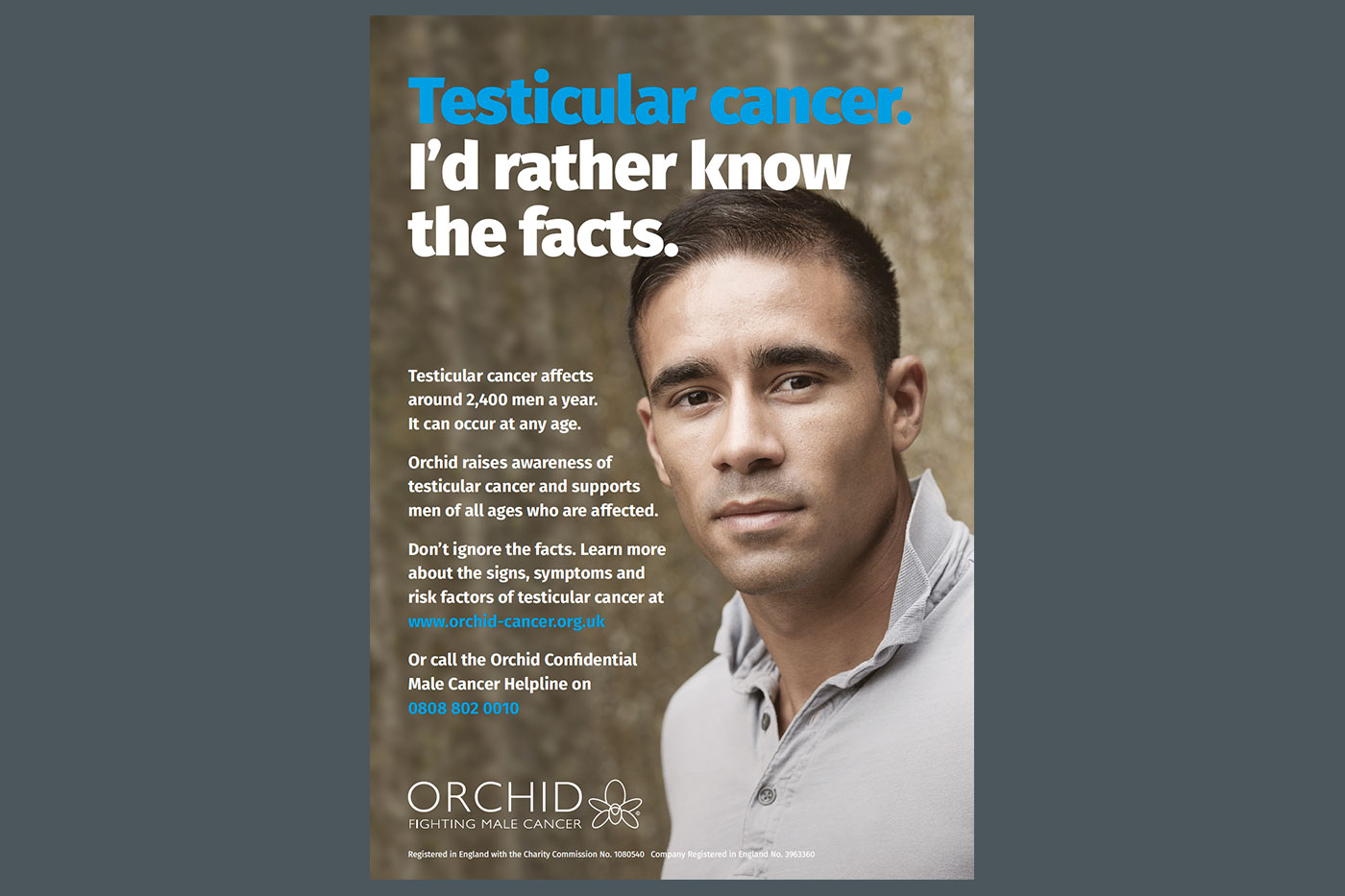
Testicular Cancer Awareness Poster
FREE
Testicular cancer awareness poster.
Click on the button below to download a PDF version
Download Testicular Cancer Awareness PosterIf you would like to order a physical copy select the quantity and then click add to basket.